Breastfeeding and Dental Health
From the early days with your newborn, breastfeeding often becomes a very important and comfortable part of your relationship with your child. As well as continuing to provide important nutrients and protection against ill health, it’s a wonderful way to continue to connect with and comfort your growing infant, both during the day and quite often at night too.In fact, night nursing is a biologically normal behaviour.
However, as time goes by and your baby’s teeth come in, a new concern may emerge. You may be told by your dentist that breastfeeding causes tooth decay and some dentists may advise early weaning from the breast, or at least no night-time nursing.
In this article we look at questions and concerns about dental health and discuss how it can be protected while you and your baby continue to enjoy your important breastfeeding relationship.
Is it true that breastfeeding will contribute to my child’s tooth decay?
Does the research show I should wean after one to prevent tooth decay?
How does diet affect dental health?
How can I ensure good dental hygiene?
What if my dentist tells me I should stop breastfeeding?
Do studies show human milk may protect against bacteria?
Are some children more susceptible to dental caries?
What can I take from all this information?
Is it true that breastfeeding will contribute to my child’s tooth decay?
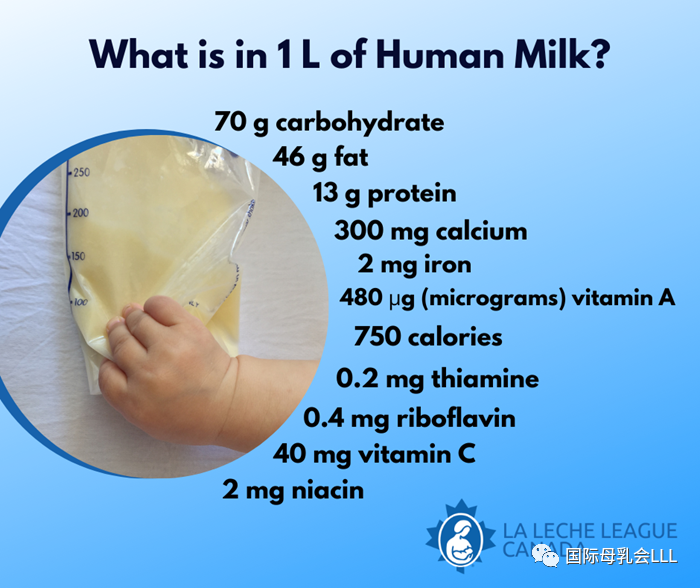
Studies show that a breastfed child is significantly less likely to suffer from tooth decay (dental caries) than a child who is formula fed. According to a report issued by the World Health Organisation (WHO) in January 2020, “Evidence suggests that infants who are breastfed in the first year of life have lower levels of dental caries than those fed infant formula.”
The report adds:“One systematic review suggested a higher risk of ECC [early childhood caries] when breastfeeding extends beyond one year of age, but the data analysis did not control adequately for important confounders such as intake of sugars from other sources.”
As well as the continuing significance to the health of mother and child, breastfeeding promotes optimal jaw and tooth development. A breastfed child is less likely to suffer from crooked teeth (malocclusion)and the longer the child is breastfed the greater the reduction in risk. A breastfed baby may also be protected from developing dental fluorosis (discolouration of teeth).
Does the research show I should wean after one to prevent tooth decay?
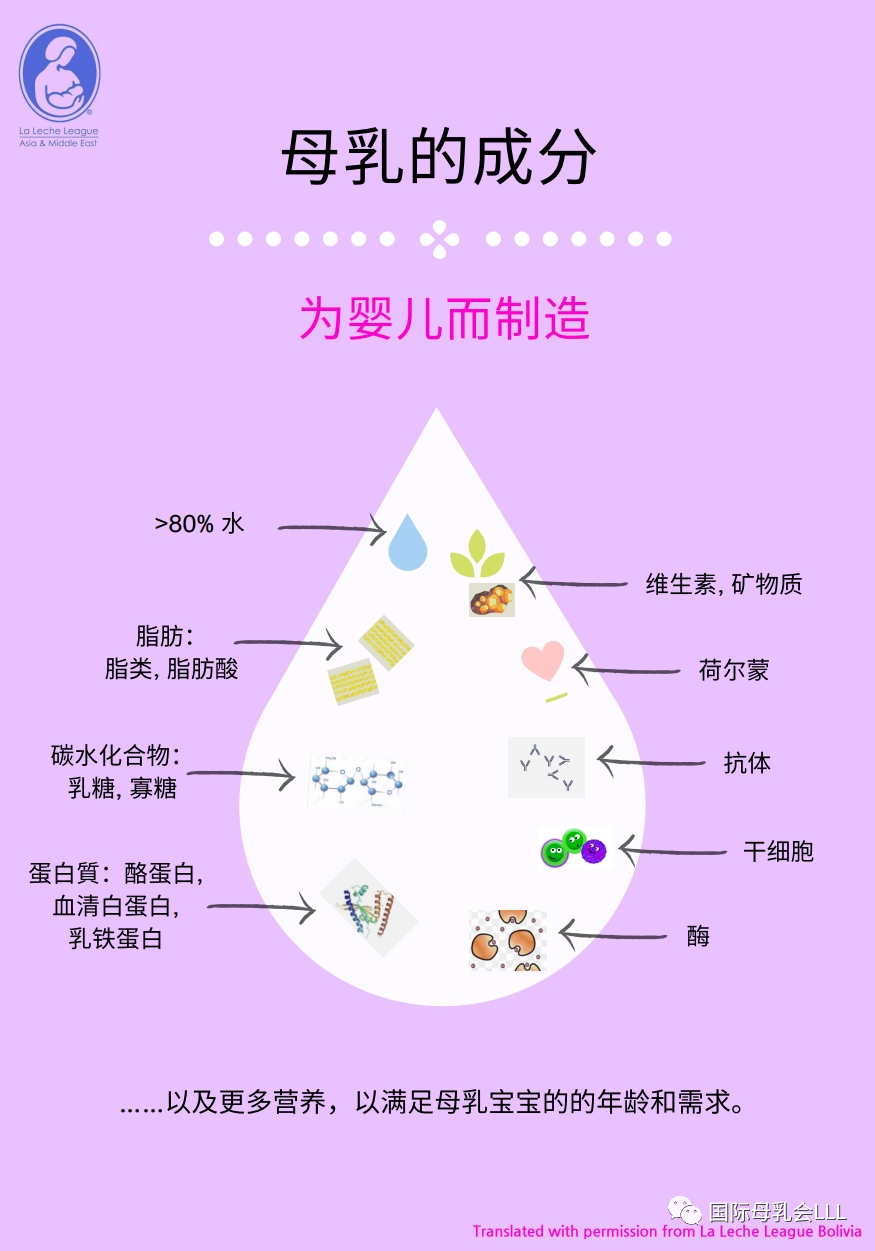
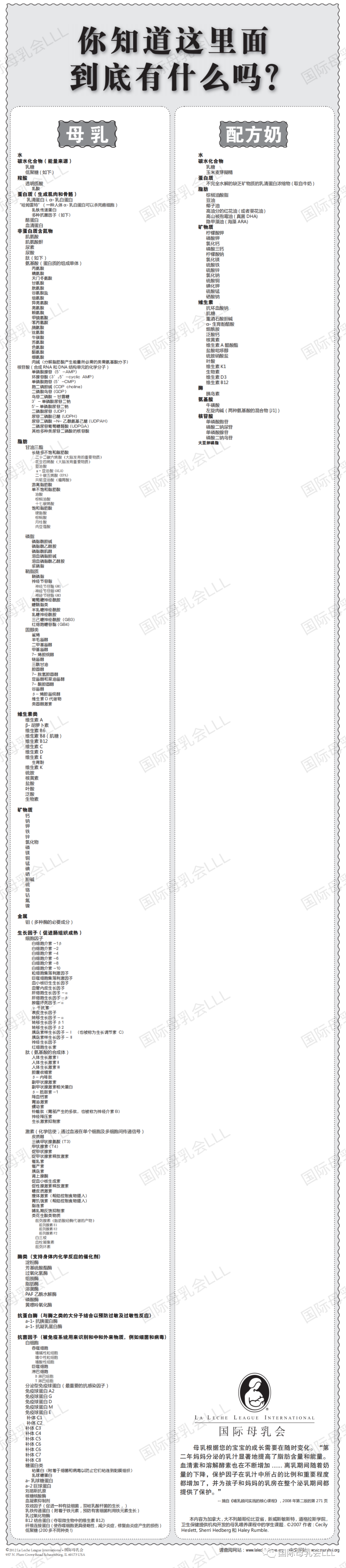
There is no convincing evidence to show that breastfeeding itself is causing problems or that stopping will prevent tooth decay. Studies often look at the effects of lactose (milk sugar, which is also present in breastmilk) on teeth, not the effects of breastmilk as a whole, with its antibacterial properties, helpful enzymes and high pH.
Research about the impact of breastfeeding on dental health after the age of one acknowledges that it is difficult to adequately control other factors such as diet, dental hygiene, and the presence of bacteria in the mouth, when looking atearly childhood caries.
In December 2018, Public Health England said that there are no good quality studies proving links between dental damage and breastfeeding beyond 12 months. Their guidance also emphasizes the risks of not breastfeeding.
Other reports agree that research may not take into account diet alongside breastfeeding. A 2019 review entitled ‘Breastfeeding and early childhood caries. Review of the literature, recommendations, and prevention’ states that results from heterogeneous studies “do not always take into account contradictory factors such as eating habits of the mother or infant (feeding during the night, number of meals per day, eating sweet foods etc.), dental hygiene, or the sociocultural context.”
Another 2019 report entitled ‘Systematic Review of Evidence Pertaining to Factors That Modify Risk of Early Childhood Caries’looked at breastfeeding and childhood caries in children aged up to 72 months. It concluded that breastfeeding for up to 24 months did not increase early childhood caries risk, although there was some “low-quality” evidence for increased risk in longer duration breastfeeding. The review added that some data indicated the impact of sugars in complementary foods increased risk.
An older US study from 2007, ‘Association between infant breastfeeding and early childhood caries in the United States’,assessed the potential risk factors for dental caries in 1,576 children aged 2-5 years old and demonstrated that there is no evidence to suggest that breastfeeding or its duration are risk factors for early childhood caries, severe early childhood caries, or decayed and filled surfaces on primary teeth.
How does diet affect dental health?
Current studies indicate that research cannot rule out our modern diet as a cause of dental problems rather than breastfeeding. Today’s diet includes many more cavity-inducing foods and it can be hard to get all those sugars off your child’s teeth.
Streptococcus mutans (S. mutans) is an oral bacterium that’s especially hard on tooth enamel in the presence of sugar. Babies can pick up S. mutans from adults who carry the strain and who share food, utensils or mouth kisses with them; therefore it is important that the primary caregiver of a baby also maintains good oral health.
Although your dentist may advise you to stop breastfeeding at night to prevent your baby or toddler from developing cavities, these factors are much more likely to play a role in your child’s dental health, making night weaning an irrelevant solution to the problem.
The importance of taking into account the overall diet of a breastfed infant is highlighted in a 2014 study from the University of California, ‘Association of long-duration breastfeeding and dental caries estimated with marginal structural models’, looking at possible links between longer-term breastfeeding and the risk of tooth decay and cavities.
Although the research found evidence of a greater risk of severe early tooth decay the more frequently a mother breastfed her child beyond the age of 24 months during the day, the author, Benjamin Chaffee, made positive comments about breastfeeding saying that the study does not suggest that breastfeeding causes caries and that the Number 1 priority for breastfeeding mothers should be ensuring their babies’ optimal nutrition.
The authors speculated that it is possible that breastmilk in conjunction with excess refined sugar in modern foods may be contributing to the greater tooth decay seen in babies breastfed the longest and most often. This study also talks about “breastmilk bottles” as opposed to breastfeeds and highlights that nearly half the children had also been given infant formula by six months.
A 2020 Australian studyalso looked at diet and dental health in pre-schoolers by studying breastfeeding patterns and the intake of free sugars in their diet. The authors concluded that “Breastfeeding practices were not associated with early childhood caries.
Given the wide-ranging benefits of breastfeeding, and the low prevalence of sustained breastfeeding in this study and Australia in general, recommendations to limit breastfeeding are unwarranted, and breastfeeding should be promoted in line with global and national recommendations. To reduce the prevalence of early childhood caries, improved efforts are needed to limit foods high in free sugars.”

How can I ensure good dental hygiene?
The overwhelming conclusion when looking at breastfeeding and dental health is that, alongside diet, dental and oral hygiene is crucial in preventing cavities.
The 2019 report entitled ‘Systematic Review of Evidence Pertaining to Factors That Modify Risk of Early Childhood Caries’concluded that “Providing access to fluoridated water and educating caregivers are justified approaches to ECC prevention. Limiting sugars in bottles and complementary foods should be part of this education.”
Chaffee, the author of the 2014 study ‘Association of long-duration breastfeeding and dental caries estimated with marginal structural models’said his team of researchers collected data on tooth brushing habits, but did not investigate a specific link between cleaning teeth after the last feeding and caries. He added that anything that removes carbohydrates and sugars from the oral cavity should help prevent tooth decay.
An often-quoted 2015 study ‘Breastfeeding and the risk of dental caries: a systematic review and meta-analysis’ commented that “There was a lack of studies on children aged >12 months simultaneously assessing caries risk in breastfed, bottle-fed and children not bottle or breastfed.”
It also concluded that when infants were no longer exclusively breastfed or formula fed, confounding factors such as diet and tooth brushing practices needed to be taken into account. The authors stated that “further research with careful control of pertinent confounding factors is needed to elucidate this issue and better inform infant feeding guidelines.”
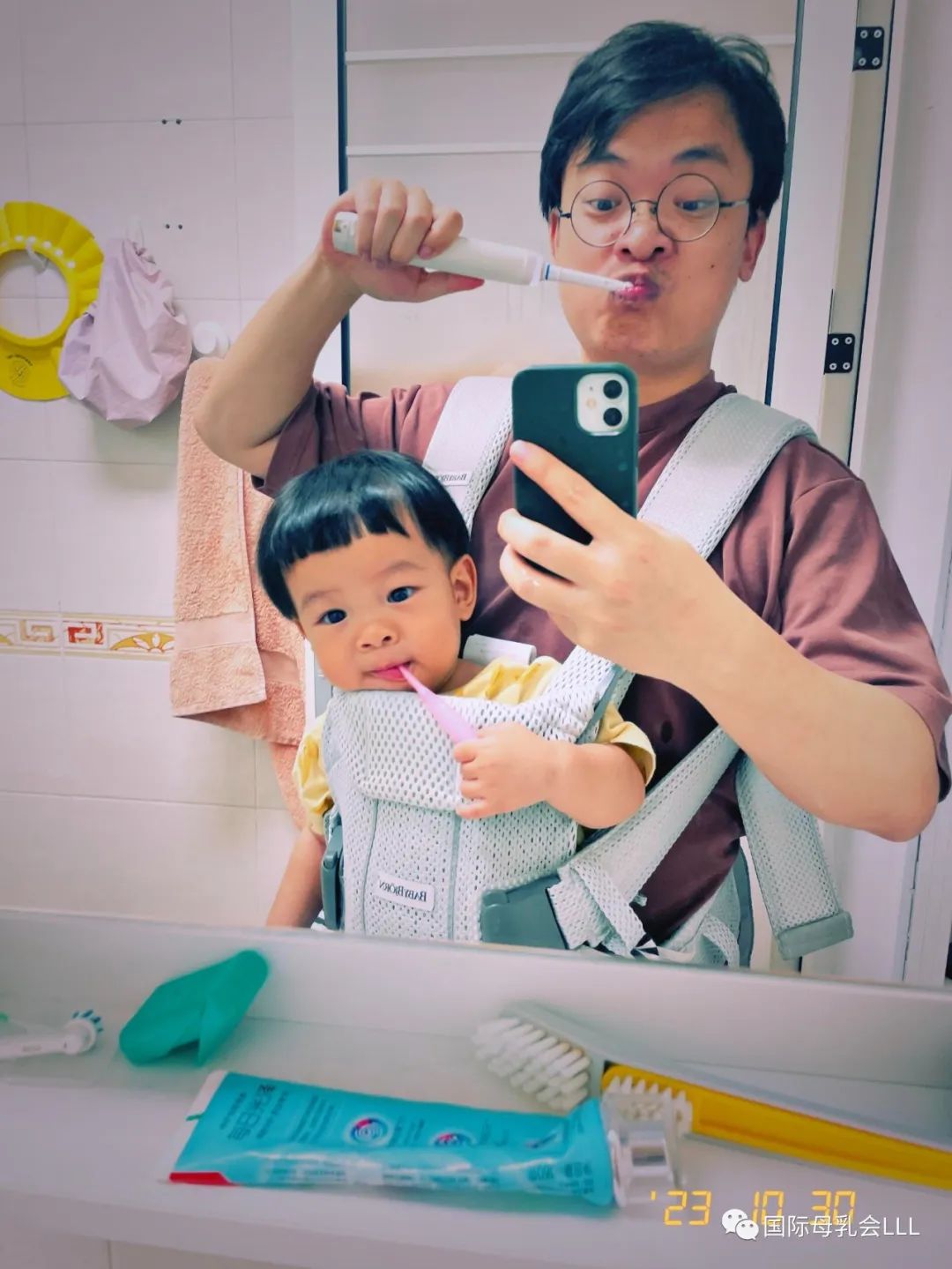
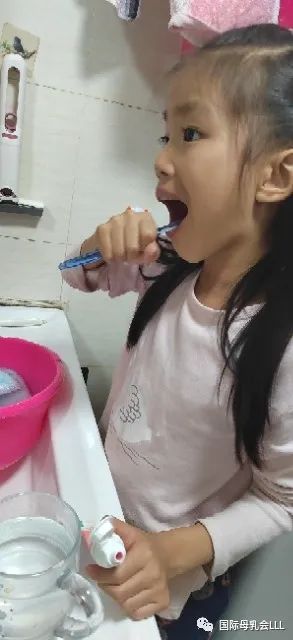
Public Health England’s recommendations are that parents or carers should brush their children’s teeth:
·as soon as they erupt;
·twice a day;
·last thing at night (or before bedtime) and on one other occasion;
·with a toothpaste containing at least 1000 ppm fluoride;
·using only a smear of toothpaste.
There seems to be general agreement that the best way to aid your child’s dental health is to brush their teeth thoroughly at least twice a day with fluoridated toothpaste. It might also help to encourage your baby to swish with, or at least sip, water after eating solid foods. Some dentists recommend wiping a child’s teeth after each nursing, including during the night, but this can prove to be a difficult and unnecessary procedure.
While there is no need to keep your child from nursing at night, it is important to brush teeth before going to sleep and not to offer any carbohydrates after that. This is in line with the findings of a 1999 study which investigated the effect of different solutions on dental health by immersing healthy, extracted teeth in them. The results showed that breastmilk alone was practically identical to water and did not cause tooth decay. However, when a small amount of sugar was added to the breastmilk, the mixture was worse than a sugar solution when it came to causing tooth decay.
You may also want to ask your dentist for information about using xylitol. This is a natural carbohydrate sugar substitute that interferes with bacteria’s ability to stick to the tooth surface. Aside from being available as a cooking ingredient, xylitol is often found in chewing gum and it’s possible that its use by mothers with high levels of S.Mutans may reduce the level of bacteria in their mouths, consequently lowering the risk of passing S.Mutans to their baby.
In summary, breastfeeding, when accompanied by toothbrushing and better nutrition by reducing the frequency and consumption of sugary foods, continues to contribute significantly to well-being for many mothers and infants. Regular consultation with a dentist for examination and preventive advice regarding dietary practices (especially sugar intake), oral hygiene, or supplementary fluoride is recommended.
What if my dentist tells me I should stop breastfeeding?
While dentists are naturally concerned about oral health, they may not have a lot of training on the overall significance of breastfeeding to the short- and long-term physical and mental health of both mother and child.
According to the 2018 Public Health England guidance on Breastfeeding and dental health, “Breastfeeding is the physiological norm against which other behaviors are compared; therefore, dental teams should promote breastfeeding and include in their advice the risks of not breastfeeding to general and oral health.”
The guidance states that dentists and their teams should support evidence-based guidelines from the WHO and the UK government and in a core message to dental teams and healthcare professionals includes the following recommendations:
·“Dental teams should continue to support and encourage mothers to breastfeed.”
·“Not being breastfed is associated with an increased risk of infectious morbidity (for example gastroenteritis, respiratory infections, middle-ear infections).”
·“Breastfeeding up to 12 months of age is associated with a decreased risk of tooth decay.”
If your dentist would like further advice, the UKHSA refers them to ‘Health Matters: Child Dental Health’ (2017)and ‘Delivering Better Oral Health: An Evidence-Based Toolkit for Prevention’ (2014).
There are supportive dentists who understand the significance of breastfeeding so if you are under pressure to wean, try to find one who respects your choices.
Do studies show human milk may protect against bacteria?
The late Dr. Brian Palmer, DDS studied children’s skulls that were thousands of years old and he found almost no cavities. In his presentations, he referred to evidence from anthropologists and commented that “If breastmilk caused decay – evolution would have selected against it. It would be evolutionary suicide for breastmilk to cause decay.”
One reason for the lack of cavities identified by Dr. Palmer may be that the mechanics of breastfeeding make it unlikely for human milk to stay in the baby’s mouth for long. During breastfeeding, the nipple is drawn deep within the baby’s mouth, and milk is literally squirted into the back of it.
The nursing child must swallow before he can go on to the next step of the suckling process. In contrast, baby bottles can drip milk, juice, or formula into the baby’s mouth even if he is not actively sucking. If the baby does not swallow, the liquid can pool in the front of the mouth around the teeth. The artificial nipple is very short, so the liquid in the bottle is likely to pass over teeth before being swallowed.
Another reason is that bacteria which cause cavity formations are inhibited by several components of human milk including high pH levels. IgA and IgG have the potential to retard streptococcal growth, and S. mutans is highly susceptible to the bactericidal action of lactoferrin, an active component of human milk.Human milk also actively strengthens teeth by depositing calcium and phosphorus on them.
Dr. Palmer was of the opinion that dry mouth is another factor that can increase the incidence of early childhood caries. Saliva, which helps maintain normal pH, is not produced as much at night, especially among those who breathe through their mouths. An infant or toddler who nurses often at night continues to produce saliva, which may help combat dry mouth.

Are some children more susceptible to dental caries?
In a survey entitled ‘Prolonged, on-demand Breastfeeding and Dental Caries – An Investigation’,Dr. Harry Torney found that four factors were significantly associated with the high caries group. The most significant relationship was with defective enamel while the other three factors related to events that had occurred while the child was in utero.
One of these was maternal stress and/or bereavement as reported by the mother. Another was a reduced intake of dairy products as estimated retrospectively by the mother. The third factor was medically diagnosed illness in the mother.
If a mother’s pre-natal diet and/or antibiotics received during pregnancy have affected the quality of a child’s tooth enamel and resistance to cavities, the permanent teeth are almost always fine. Diet and oral hygiene are also factors, as confirmed by the more recent research discussed above.
Dr. Torney found no correlation between the onset of dental caries under two years of age and breastfeeding patterns such as feeding to sleep, frequent night feeds, etc. In his opinion, under normal circumstances, the antibodies in breastmilk counteract the mouth bacteria which cause tooth decay.
However, in the presence of small enamel defects, the teeth become more vulnerable, and the protective effect of breastmilk is not sufficient to counteract bacteria combined with the sugars in the milk.
According to this research, a baby who is exclusively breastfed (no supplemental bottles, juice, or solids) will not have decay unless he is genetically predisposed, i.e. soft or no enamel. In a baby who does have a genetic problem, weaning will not slow down the rate of decay and may speed it up due to lack of lactoferrin.
Dr. Palmer’s research is in line with this: “Human milk alone does not cause dental caries.
Infants exclusively breastfed are not immune to decay due to other factors that impact the infant’s risk for tooth decay. Decay causing bacteria (streptococcus mutans) is transmitted to the infant by way of parents, caregivers, and others.
A couple of studies have also highlighted a possible association between early childhood caries and maternal Vitamin D deficiency during pregnancy.
What can I take from all this information?
While you may initially feel concerned about the effects of longer-term and nighttime breastfeeding, it is important to look at all the factors contributing to the dental health of your breastfed child.
Historically children who nursed all night had little or no decay until the advent of decay-inducing foods.
Human milk alone rarely contributes to decay and actually has tooth-strengthening properties.
While parents need to be aware of the dangers of sweet foods and drinks and of the benefits of strict oral hygiene and visits to the dentist, it’s important not to overlook the impact on physical and emotional health of breastfeeding for the baby, family and society as a whole.
The WHO recommends that infants be exclusively breastfed for the first six months of life to achieve optimal growth, development and health and then continue breastfeeding for up to two years of age and beyond, alongside complementary foods.
When using the evolution of other primates as a comparison point for humans, it is interesting to notice that in human babies breastfeeding would be expected to continue for at least two and a half years.
Anthropologist Kathy Dettwyler states that while“it is meaningless, statistically, to speak of an average age of weaning world- wide” anthropologists have found that children naturally wean between two and a half years and around seven years of age.
Weaning from the breast before you and your baby are ready because of unsubstantiated fears of tooth decay would be denying both of you of the many positive outcomes from continued breastfeeding and may lead to the unnecessary introduction of bottles.
The research discussed above shows that there is no need to night wean your child to take care of their dental health. Adopting a good oral hygiene regimen, using fluoridated toothpaste and consuming a low-sugar diet are likely to have a much more significant impact in terms of reducing the risk ofearly childhood caries.

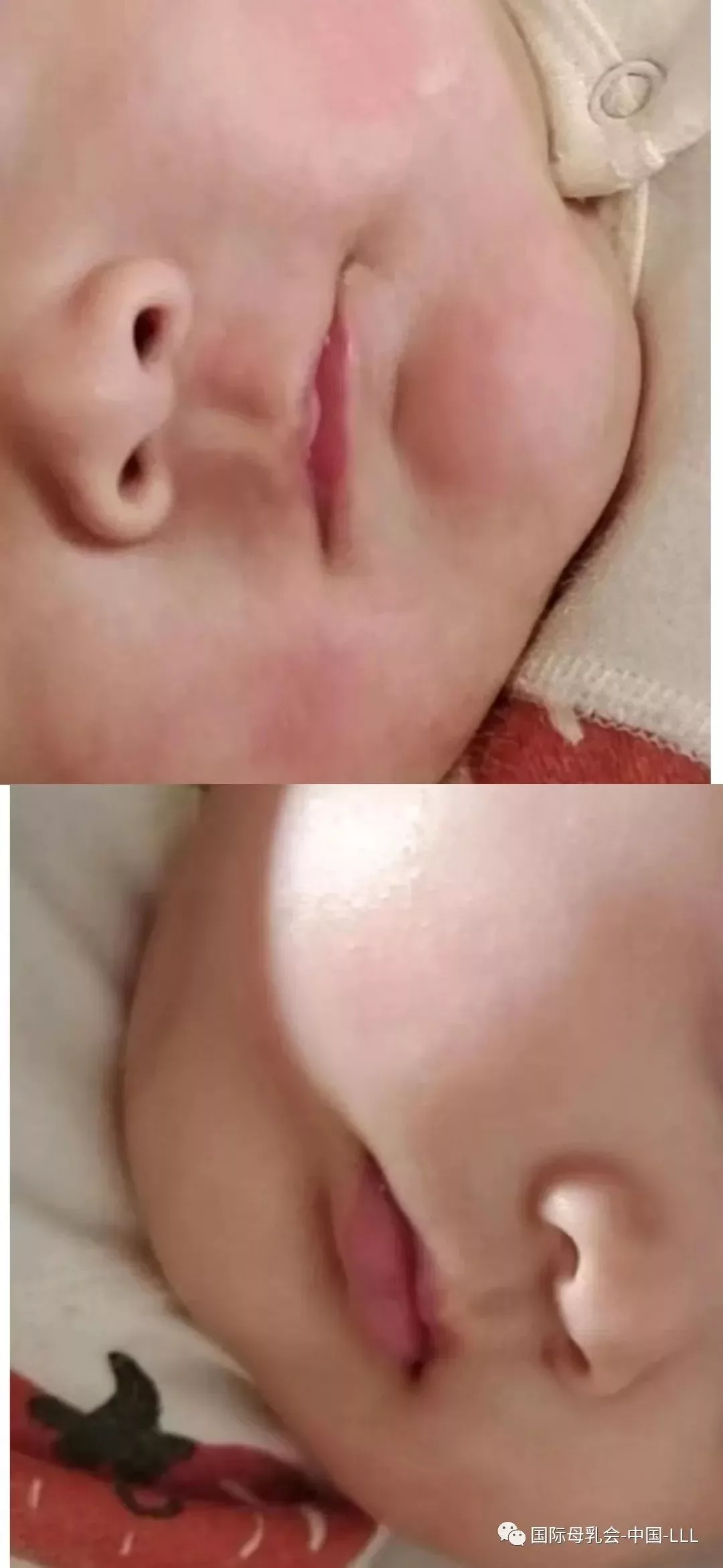
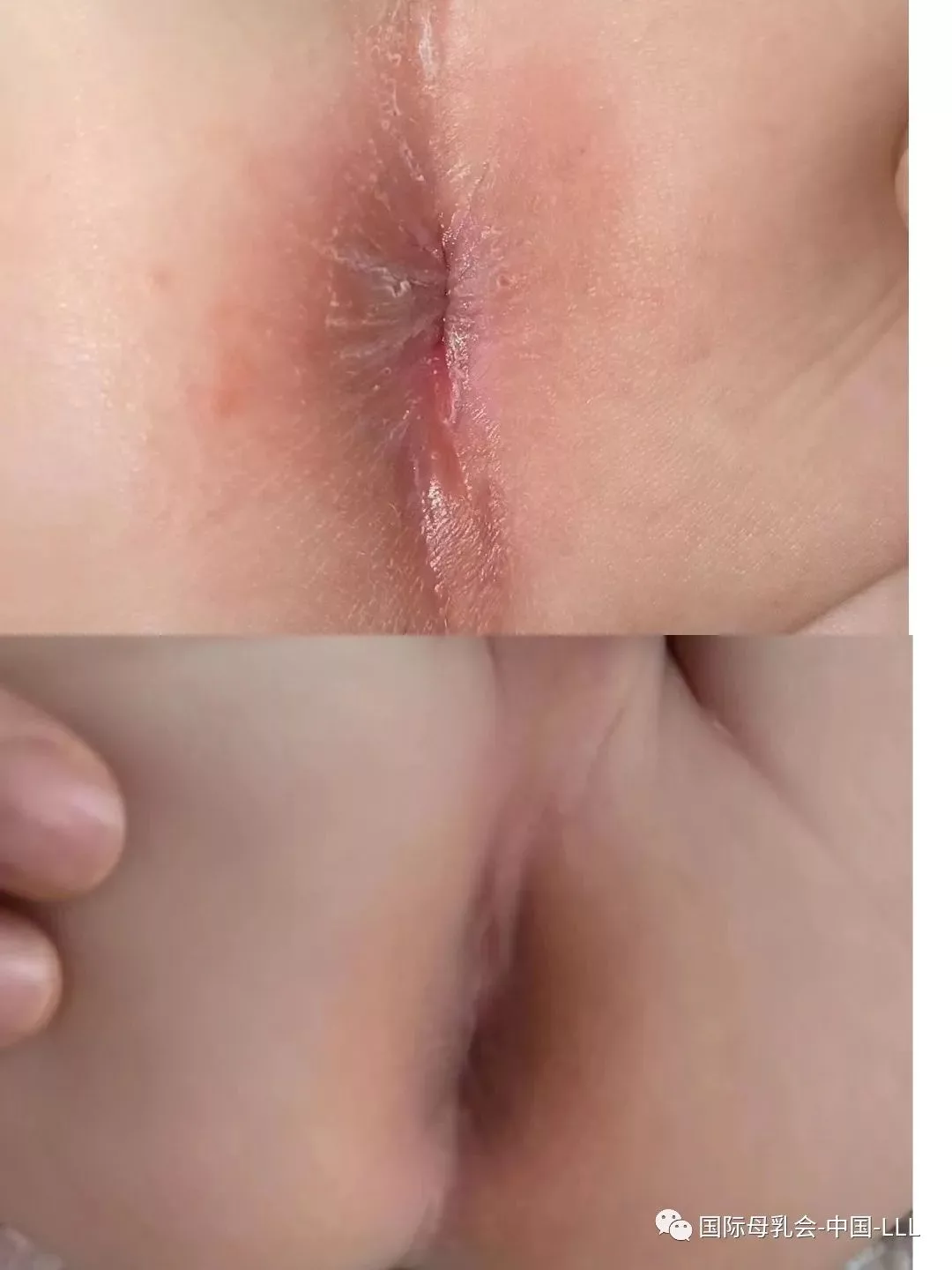
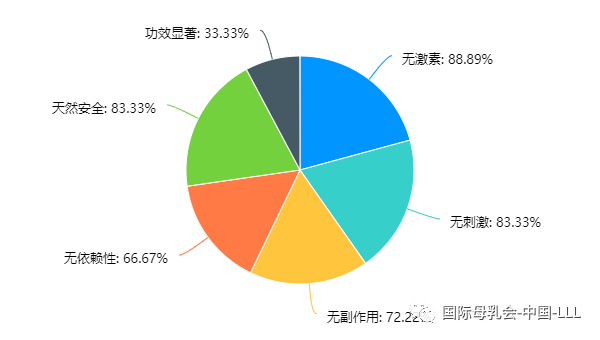
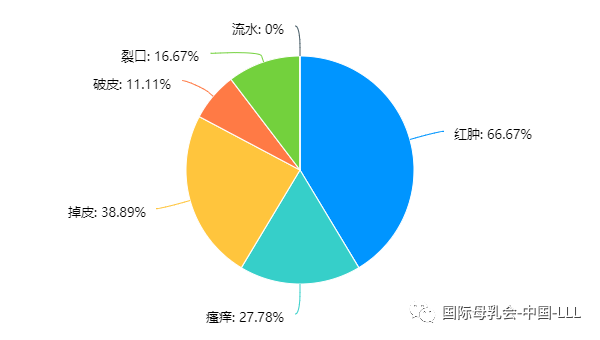 使用奇异佳修护霜后明显改善的皮肤问题
使用奇异佳修护霜后明显改善的皮肤问题