点击上方国际母乳会LLL 设为星标,获取哺乳信息

什么是正常的婴儿黄疸 ?
黄疸
即皮肤、巩膜(俗称“眼白”)、牙龈和嘴唇内侧发黄,在母乳宝宝中很常见也很正常。
发黄:是由于婴儿血液中的胆红素过多引起的。
而胆红素是由红细胞破坏时产生的。在子宫里,胎儿需要有较多的红细胞,才能把氧气从胎盘输送到全身。
婴儿一出生,就开始用肺呼吸来获得氧气,不再需要体内这些多余的红细胞了。它们分解后在婴儿体内循环,其中一个代谢产物是一种黄色色素,叫做胆红素,它可以通过粪便自然地从婴儿体内清除。
第一次的排便(即胎便)含有大量胆红素,所以它是黑色的。出生后的头几天婴儿吃得越多,胆红素从婴儿体内排出的速度就越快。大部分胆红素(98%)会通过婴儿早期的排便清除掉。肤色较深的婴儿可能不会显现黄疸引起的发黄,所以更应该仔细观察。
胆红素值上升缓慢,通常在出生后第3~5天达到峰值,不超过12毫克/分升 (你的奶量通常也会在产后第3~5天急剧增加。如果婴儿吃奶很好,就会更频繁、大量地排便)。
除了频繁有效地哺乳之外,轻度黄疸通常不需要治疗,可自行消退。摄入足够奶量就有助于婴儿清除体内的胆红素。胆红素水平的轻度升高,在有些婴儿中可能会持续15周或更长时间。
喂养不足型黄疸:
当婴儿没有吃到足够的初乳/母乳来清除胆红素时,就会产生喂养不足型黄疸。
胆红素就无法尽快被清除掉,它会被婴儿的肠道吸收,重新回到血液中,使它达到更高的水平。这会导致婴儿的皮肤和眼睛更黄。
皮肤颜色较深的婴儿可能无法识别出发黄的加重。检查牙龈和嘴唇内侧有助于识别。
婴儿可能会越来越嗜睡,使得喂奶变得更难。 医护人员会监测婴儿的胆红素水平。让婴儿多吃奶至关重要!黄疸较重时,通常需要照蓝光来辅助解决问题。
有时黄疸会一直持续到出生两周以后。这通常被称为延迟性、迟发性或母乳性黄疸。
表征:
中度升高的胆红素水平有时会在婴儿体内维持数周时间。这在出生后早期胆红素水平较高的婴儿中更为常见。迟发性黄疸的婴儿通常反应和吃奶都很好、体重增长和发育也正常。
只要胆红素水平不超过20毫克/分升,延迟性黄疸无需任何治疗就会在12~15周左右消退。
一些医疗保健人员会建议暂停母乳,但这既没有好处,也没有必要。(请参阅下列关于黄疸管理的母乳喂养医学会第22号临床指南,这是可以分享给医疗保健人员的相关信息)。
英文版本:www.bfmed.org/assets/DOCUMENTS/PROTOCOLS/22-jaundice-protocol-english.pdf
中文(繁体字)版本:www.bfmed.org/assets/DOCUMENTS/PROTOCOLS/22-Jaundice-17-1.pdf
有时是。但轻中度的黄疸并不危险。胆红素是一种强效抗氧化剂,在保护新生儿健康方面起着重要而有益的作用。
然而如果胆红素水平过高,就会损伤婴儿的大脑(译者注:Kernicterus或核黄疸)。安全的胆红素水平要根据胎龄、体重以及婴儿整体的健康状况来综合确定。较小的婴儿或早产儿所能耐受的胆红素水平比足月儿还低,所以更有脑损伤的风险。
如果足月儿在出生后的第一个24小时内就出现黄疸、快速上升,并超过17毫克/分升,说明存在更严重的问题。有时这被称为病理性黄疸,这通常不是母乳不足的缘故,而是由其它因素引起的。需要在不中断母乳喂养的情况下及时进行评估和治疗。
新生儿黄疸的危险因素:
男孩比女孩更容易发生黄疸。亚洲婴儿出现黄疸的可能性最大,其次是北美土著婴儿、白种人婴儿、最后是美籍非裔婴儿。O型血和RH阴性血母亲的婴儿更可能有黄疸。
*尽早、频繁地母乳喂养。
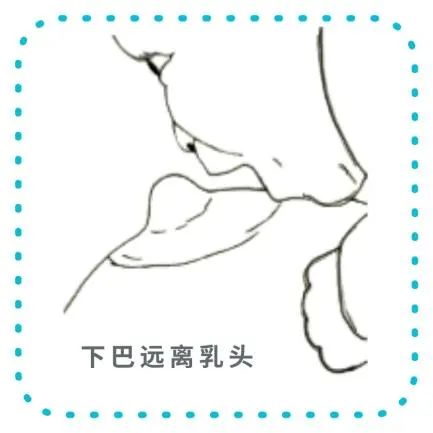
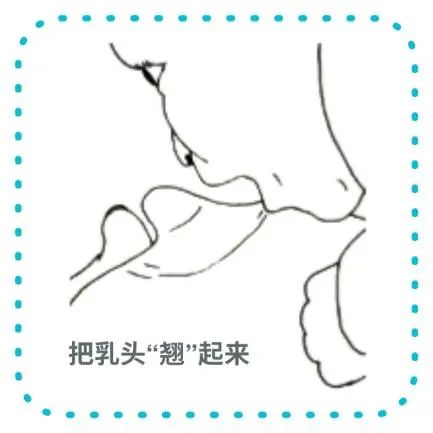
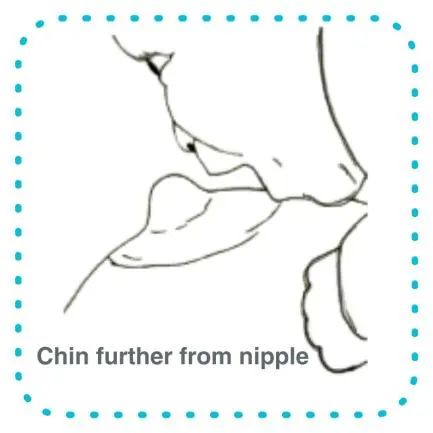
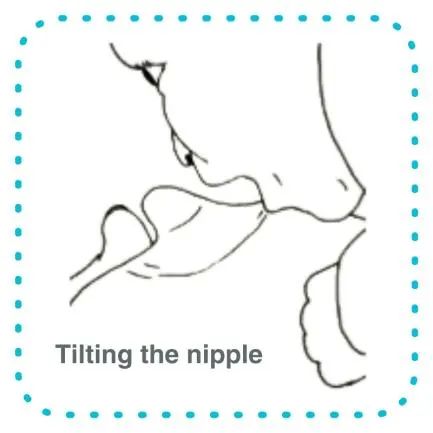
分娩后尽快开始母乳喂养。良好的含乳对于有效排出乳汁非常重要。请参阅哺乳姿势和含乳姿势这两篇文章。尽早哺乳可以帮助婴儿早点排出胎便(也就是第一次大便)。
*用舒服的半躺姿势。
垫好你的腰背,抱着婴儿皮肤贴着皮肤、胸贴着胸。半躺式哺乳姿势可以让婴儿用他天生的反射找到乳房并含乳,这也解放了你的双手,便于你在需要时帮助他。你和宝宝可以用这种姿势哺喂很多日子,这有助于你们彼此了解,并学会如何含好乳房。产后初期要持续频繁地把婴儿抱到你的胸前,并对所有的哺乳信号做出回应。
*避免给婴儿喝水或葡萄糖水。
这不仅不会预防黄疸或降低胆红素水平,反而会妨碍婴儿吃到足够的母乳。
*婴儿出院后的两天内,安排一次医疗保健人员的家访。
*如果婴儿出现以下情况,请咨询医护人员:
– 嗜睡
– 吃奶不好
– 排便少于预期
PS:嗜睡和吃奶不好是黄疸值增高的征兆。
胆红素水平可通过验血测得。如果婴儿存在下列情况,医护人员可能会要求验血:
-
婴儿嗜睡,并且吃奶不好
-
婴儿身体的很多部位看起来很黄
-
婴儿的皮肤和眼睛在出生后24小时内就开始发黄
治疗严重的黄疸可能需要婴儿照一段时间蓝光。这种特殊的光有助于分解胆红素,然后通过婴儿的尿液和大便排出体外。
照蓝光时,需要遮住婴儿的眼睛。治疗过程中母婴分离会令人不安。你可以和婴儿待在一起,大多数情况下,也可以把婴儿从蓝光箱中抱出来哺乳(译者注:目前国内也有一些开展蓝光治疗而不需要母婴分离的医疗机构)。喂奶时和婴儿做肌肤接触可以激发出他本能的哺乳行为,也能让你自己平静下来。
婴儿也可能需要添加挤出的母乳、捐赠的母乳或配方奶。如果他嗜睡且吃奶不好,补充喂养就很有必要。如果你的泌乳量增长缓慢,也有必要补充喂养。婴儿得靠进食才能清除胆红素。如果婴儿在乳房上吃不到足够的母乳,就需要添加奶以清除体内的胆红素。你可以用杯子、勺子、乳旁加奶或奶瓶来添加。
高胆红素血症的治疗通常需要几天时间。重要的是在这段时间里要挤奶,这样你才能为婴儿提供自己的母乳,并建立起充足的奶量。请参阅建立奶量和如何挤奶。胆红素水平一旦下降,婴儿就会变得更机警、哺乳也会改善。
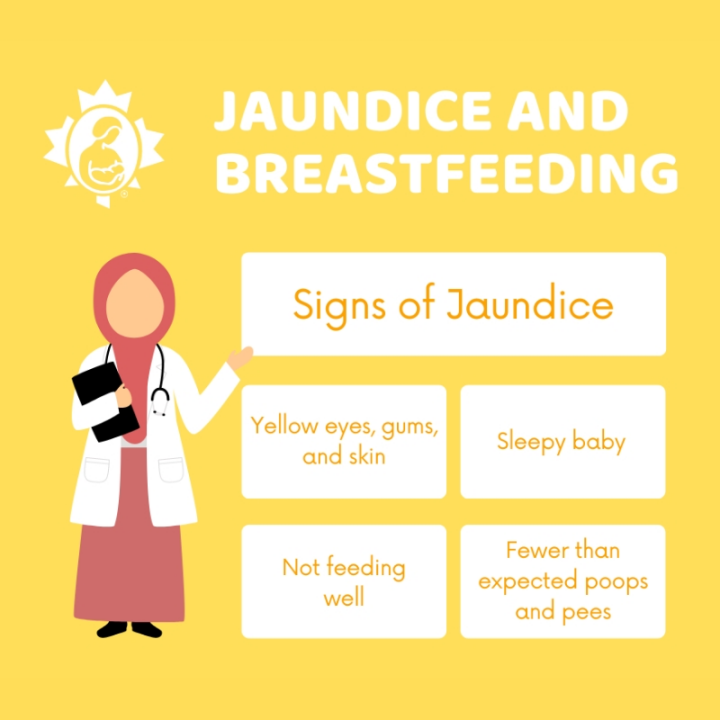
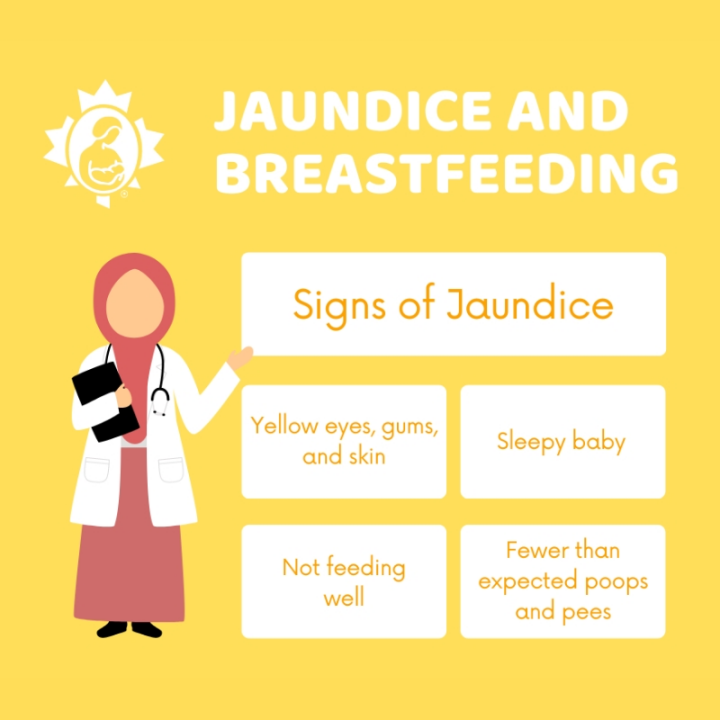
Jaundice and Breastfeeding
What is normal infant jaundice?
Jaundice, yellowing of the skin, eyes, gums and inner lips, is common and normal in breastfeeding infants. The yellow colour is caused by extra bilirubin in the baby’s blood. Bilirubin is produced when red blood cells break down. In the womb, your baby has extra red blood cells to bring oxygen from the placenta. Once your baby is born, he uses his lungs to get oxygen. These extra blood cells are no longer needed.
They break down to be recycled in your baby’s body. One byproduct is a yellow pigment called bilirubin. It is removed naturally from your baby’s body in the stools (poops). The first stool, meconium, has a large amount of bilirubin. This is why it is black in colour. The more your baby feeds in the early days, the quicker the bilirubin leaves your baby’s body. Most of the bilirubin (98%) will be eliminated in your baby’s early stools. Babies with darker skin tones may not show the yellowing effect of jaundice, so they should be observed carefully.
Normal, mild jaundice generally takes a few days to appear. The level rises slowly, usually peaking between days 3 and 5 at less than 12 mg/dl. (Between days 3 and 5 is also when your milk production should increase dramatically. When your baby is feeding well, this results in more frequent and larger poops.) Mild jaundice usually resolves without treatment other than frequent and effective feeding. Adequate milk intake is what helps your baby clear the bilirubin from his body. Some babies will have mildly elevated bilirubin levels for as long as 15 weeks or longer.
What is suboptimal intake jaundice?
Suboptimal intake jaundice occurs when a baby is not getting enough colostrum/milk to eliminate the bilirubin. When there is not enough milk intake, bilirubin is not eliminated as quickly as it should be. If the bilirubin is not eliminated quickly, it is absorbed from your baby’s gut back into the blood at higher levels. This causes more yellowing of your baby’s skin and eyes. This increase in yellowing may not be recognized in a baby with darker skin colour. It’s helpful to check the gums and inner lips. Your baby may become more and more sleepy, making feeding even more challenging. Your baby’s bilirubin levels will be monitored by your healthcare provider. It is essential that your baby gets more to eat. Phototherapy treatment is often required to help settle things down.
What is prolonged (late-onset) jaundice?
Sometimes jaundice lasts beyond the first two weeks of life. This is often called prolonged, late-onset, or breast milk jaundice. Bilirubin can sometimes remain in your baby’s body at moderate levels for many weeks. This is more common in babies who had higher bilirubin levels earlier. Babies with late-onset jaundice are alert, feeding well, gaining weight and growing. As long as bilirubin levels stay below about 20 mg/dL, prolonged jaundice resolves without any treatment by about 12 to 15 weeks. Some healthcare professionals may recommend temporary weaning, but this is not beneficial or necessary. (For information to share with your healthcare provider, see Academy of Breastfeeding Medicine Protocol #22 Jaundice: www.bfmed.org/assets/DOCUMENTS/PROTOCOLS/22-jaundice-protocol-english.pdf).
Is jaundice dangerous?
Sometimes it is. But mild to moderate jaundice is not dangerous. Bilirubin is a powerful antioxidant and can play an important and beneficial role in protecting newborn health.
However, if bilirubin reaches too high a level, it can cause injury to a baby’s brain. Safe bilirubin levels are determined individually based on gestational age, weight and your baby’s overall health. Small or premature babies are at risk of brain injury from a lower level of bilirubin than can be tolerated by a full-term baby.
Jaundice that appears within the first 24 hours, rises quickly, and reaches higher than 17 mg/dl in a full term baby is indicative of a more serious problem. This is sometimes called pathological jaundice. This is often caused by other factors, not a lack of milk. It needs to be assessed and treated promptly without interrupting breastfeeding.
Risk factors for jaundice in newborns
· Delayed milk production. There are many reasons why breastfeeding might get off to a slow start. Cesarean section birth and first time pregnancy are two common situations where it helps to take extra care with getting breastfeeding established.
· Premature birth.
· Birth earlier than 38 weeks.
· Small for the baby’s gestational age.
· Bruises in the baby’s head from the birth.
· Maternal diabetes.
· Rh sensitization.
· Family history of jaundiced infants.
Boys are more likely to be jaundiced than girls. Asian babies are most likely to be jaundiced, followed by Indigenous North American babies, Caucasian babies and finally African American babies. O blood type and RH negative mothers are also more likely to have jaundiced babies.
Preventing high jaundice levels
· Breastfeed early and frequently. Start as soon after birth as possible. A good latch is important for effective milk removal. See Positioning and Latching. Early feedings help your baby pass the meconium or first stool quickly.
· Lie-back in a comfortable, reclined position that supports your back. Hold your baby skin to skin and chest to chest. The laid-back position allows your baby to use her inborn reflexes to find the breast and latch. It also frees your hands so you can help, as needed. You and your baby can feed like this for many days. It will help you get to know each other and learn how to get a good latch. Continue putting your baby to breast frequently in the early days. Respond to all feeding cues.
· Avoid giving your baby water or glucose. This will not prevent jaundice or bring down bilirubin levels. It will interfere with your baby getting enough milk.
· Arrange a visit with your baby’s healthcare provider within two days of discharge from a hospital birth.
· Consult your baby’s healthcare provider if your baby is:
Ø sleepy.
Ø not feeding well.
Ø not pooping as expected.
Sleepiness and poor feeding are signs of high jaundice levels.
Treatment for jaundice
Bilirubin levels are checked by a blood test. Your baby’s healthcare provider may order a blood test if:
· your baby is sleepy and not feeding well.
· much of your baby’s body looks yellow.
· your baby’s skin and eyes started turning yellow within the first 24 hours.
Treatment of severe jaundice may require your baby to spend time under phototherapy lights. These special lights help break down the bilirubin so it can be removed in your baby’s urine as well as the stool. Your baby’s eyes are covered while under these lights. Separation during this treatment can be upsetting. You can stay with your baby, and in most cases, take your baby out from under the lights to feed. Placing your baby skin to skin during these feedings encourages instinctive feeding behaviours. Holding your baby skin to skin also calms you.
Your baby may also require supplementation with expressed milk, donor milk or formula. This may be necessary if your baby is sleepy and not feeding well. It may also be necessary if your milk production is slow to increase. Your baby needs food to eliminate the bilirubin. If your baby is not getting enough milk at breast, supplementation is needed to remove the bilirubin from your baby’s body. You could supplement with a cup, spoon, at-breast supplementer or bottle. See How to Protect Breastfeeding while Supplementing (https://www.lllc.ca/how-protect-breastfeeding-while-supplementing) .
Treatment of high bilirubin levels usually takes a few days. It is important to express your milk during this time so that you can provide your own milk for your baby and establish a plentiful milk supply. See Establishing Your Milk Supply and Expressing Your Milk. Once your baby’s bilirubin levels are dropping, your baby will be more alert and will feed better.
If you have any breastfeeding questions or concerns, contact your local La Leche League China Leader who can provide you with support and information.
Updated 2022
参考文献References
Flaherman, V.J., Maisels, M.J. and the Academy of Breastfeeding Medicine. (2017). ABM Clinical Protocol #22: Guidelines for Management of Jaundice in the Breastfeeding Infant 35 Weeks or More of Gestation—Revised 2017, Volume 12, Number 5, 2017. DOI: 10.1089/bfm.2017.29042.vjf
Mohrbacher, Nancy. (2020). Breastfeeding Answers: A Guide for Helping Families, Second Edition. Nancy Mohrbacher Solutions, Inc., 245-246.
资料来源Source
https://www.lllc.ca/jaundice-and-breastfeeding
作者:加拿大母乳会
翻译:传艳
审核: Lynn 、Marien、楠楠
编辑:沐凡
微信公众号|视频号|小红书|抖音|新浪微博|今日头条|哔哩哔哩|腾讯视频|优酷
搜索关键字“国际母乳会LLL”
更多阅读资料,
欢迎大家访问“国际母乳会LLL”官网:
https://www.muruhui.org/







 可以让更多的妈妈和婴儿获益!
可以让更多的妈妈和婴儿获益!